Insurer Seeks to Void $3.35B Stamp Inventory Policy Over Alleged Misrepresentation

February 16, 2026 | JacobiJournal.com — A New York federal court is reviewing a high-stakes insurance dispute after a stamp dealer filed a $3.35 billion stamp insurance claim for inventory lost in a fire. The insurer has challenged the claim, arguing that the dealer misrepresented the value of its collection when applying for coverage, and is asking the court to declare the policy void from inception. The case has drawn attention in both legal and collectibles circles because of the unprecedented scale of the claim and the potential implications for insurance coverage of high-value items. Experts note that if the insurer prevails, it could reshape how stamp dealers and other collectors document and disclose inventory for insurance purposes. Legal analysts also highlight the intersection between insurance law and fraud allegations. Courts often weigh the intent behind value declarations when evaluating whether misrepresentation occurred, making this stamp insurance claim a critical reference point for future high-value collectible cases. What Happened With the Stamp Collection Claim? The stamp dealer reported the destruction of a substantial inventory in a recent fire, prompting the $3.35 billion stamp insurance claim. The insurer alleges that the company inflated the value of its collection when purchasing the policy, claiming this misrepresentation directly affected underwriting decisions. According to the insurer, accurate valuation disclosures are crucial, particularly in policies covering rare collectibles with potentially billions in market value. If the dealer intentionally overstated inventory worth, the insurer argues that the coverage should never have been issued or should have carried different terms. The court complaint details the insurer’s request to invalidate the policy retroactively. This legal strategy, if successful, would negate the dealer’s claim entirely and highlight the legal consequences of inaccurate reporting in high-value insurance applications. How the Insurer Justifies Policy Voidance The insurer contends that underwriting for high-value collectibles relies heavily on precise valuations. When applicants misstate inventory values, insurers face disproportionate risk, potentially resulting in massive payouts like the $3.35 billion stamp insurance claim. Legal filings suggest the insurer is asserting that misrepresentation, if proven, constitutes fraud under state and federal law. This approach not only challenges the claim but also seeks to recover premiums or adjust the terms retroactively, a common tactic in disputes involving valuable assets. Experts point out that this strategy also sends a warning to other collectors: misrepresentations or omissions on insurance applications can lead to full denial of claims, policy voidance, and potential civil liability for fraud, even in high-stakes markets like rare stamps. Why This Case Matters to the Insurance Industry This case underscores the complexities insurers face when covering rare collectibles. A $3.35 billion stamp insurance claim represents a unique exposure for underwriters, emphasizing the need for stringent documentation, third-party appraisals, and careful assessment of reported values. Insurance attorneys note that the outcome could influence industry standards, encouraging stricter auditing and verification procedures before issuing coverage. Insurers may require more detailed inventories, photographs, and independent appraisals to mitigate risk. Additionally, the case highlights the broader legal and regulatory implications. Fraud allegations in high-value claims can attract scrutiny from regulators, potentially affecting compliance requirements, reporting standards, and even future policyholder eligibility. Where to Find Official Court Filings Readers can access court documents and complaints through the United States District Court for the Southern District of New York or via reliable legal reporting systems. Reviewing filings provides insight into both the insurer’s arguments and the dealer’s responses regarding the stamp insurance claim. Official sources like PACER allow attorneys, claims professionals, and researchers to track case developments in real time, ensuring accurate information for industry analyses and med-legal commentary. Monitoring these filings can also help legal professionals anticipate potential precedents and understand how courts evaluate alleged misrepresentation and fraud in high-value insurance cases. FAQs: About the Stamp Insurance Claim What does it mean for an insurance policy to be void from inception? A policy voided from inception is treated as though it never existed due to misrepresentation, fraud, or material nondisclosure during application. How do insurers verify high-value collectibles before approving coverage? Insurers typically require independent appraisals, detailed inventories, and historical documentation to confirm the authenticity and value of high-value collectibles. Why is this $3.35 billion claim significant for the collectibles market? The size of the claim underscores the financial exposure for insurers covering rare and high-value assets, highlighting the importance of accurate valuation and disclosure. What legal consequences can arise from misstating inventory values? Misrepresentation can result in denied claims, policy voidance, civil liability, and potential criminal fraud charges. Stay informed on high-value collectibles and insurance fraud developments. Subscribe to JacobiJournal.com for timely legal analysis and investigative reporting. 🔎 Read More from JacobiJournal.com:
Lindberg Ordered to Pay $526 Million in Fraud Case Brought by Insurers

February 9, 2026 | JacobiJournal.com — A North Carolina trial court has ordered convicted insurance executive Greg Lindberg and two affiliated companies to pay more than $526 million to a group of insurers, concluding that the businesses were fraudulently induced to financially support Greg Lindberg-controlled entities to their own detriment. The ruling represents one of the largest civil fraud judgments involving the insurance industry in recent years and adds to Lindberg’s mounting legal exposure following prior criminal convictions. What the Court Found in the Insurers’ Fraud Claims The court determined that Greg Lindberg orchestrated a scheme in which insurers were misled into providing capital support under false pretenses. According to the findings, the financial backing was presented as necessary to stabilize related enterprises, while material risks and conflicts were concealed. Evidence presented at trial showed that the transactions disproportionately benefited Lindberg-controlled companies while exposing insurers to losses that were neither adequately disclosed nor justified by legitimate business needs. Why the Judgment Reaches Half a Billion Dollars The $526 million award reflects a combination of compensatory damages tied to insurer losses and additional amounts linked to the severity and scope of the misconduct. The court emphasized that the fraudulent inducement was systemic rather than isolated, affecting multiple insurers over an extended period. Judges also pointed to the misuse of corporate control and insider influence as aggravating factors supporting the size of the judgment. How This Case Fits Into Greg Lindberg’s Broader Legal Troubles Greg Lindberg, once a powerful figure in the insurance and financial services sector, has faced years of scrutiny from regulators and prosecutors. The civil ruling follows earlier criminal proceedings and underscores how civil fraud liability can persist independently of criminal sentencing. Legal analysts note that insurer-initiated fraud litigation has become more aggressive in recent years, particularly where policyholder stability and reserve integrity are implicated. What This Means for the Insurance Industry The decision sends a clear warning to executives and controlling shareholders that courts will closely examine insider transactions that place insurers at risk. For carriers, the case highlights the importance of governance safeguards, transparency in capital transactions, and early detection of coercive or deceptive financial arrangements. For regulators and policyholders, the ruling reinforces the judiciary’s willingness to impose substantial financial consequences for abuse of insurer assets. Readers can review public information on insurance fraud enforcement and civil remedies through the North Carolina Judicial Branch. FAQs: Fraud Judgment Against Greg Lindberg Who is Greg Lindberg? Greg Lindberg is a former insurance executive and entrepreneur who previously controlled multiple insurance-related companies. He has been involved in both criminal and civil legal proceedings related to his business practices. Over the years, Lindberg has drawn regulatory scrutiny and litigation attention for actions affecting insurers and investors. Why were insurers awarded damages? Insurers were awarded damages because the court found they had been deliberately misled into providing financial support to Lindberg-controlled entities. The representations made to the insurers concealed material risks and conflicts of interest, resulting in significant financial losses. The judgment reflects the court’s determination that the inducement was fraudulent and caused measurable harm to the companies involved. Does this judgment relate to criminal charges? No, this ruling is a civil fraud judgment and is separate from any prior criminal proceedings. While it arises from related conduct, it specifically addresses financial losses suffered by insurers due to deceptive practices. Criminal liability and civil liability are distinct, meaning that even after criminal convictions, Lindberg can still be held accountable in civil court. Can insurers still recover the full amount awarded? Recovery of the $526 million award will depend on several factors, including the availability of Lindberg’s personal and corporate assets, the success of any enforcement actions taken by the insurers, and the outcome of potential appeals. While the court has issued a judgment in favor of the insurers, collecting the full amount can be a complex process that may take months or even years. Asset tracing, garnishments, or other collection mechanisms may be required to secure payment. Subscribe to JacobiJournal.com for in-depth reporting on fraud, financial crime, and high-stakes civil litigation. 🔎 Read More from JacobiJournal.com:
California Insurance Fraud Investigations Mark 90 Years of Consumer Protection

February 2, 2026 | JacobiJournal.com — For nine decades, California’s regulators have led the fight against insurance fraud, protecting consumers from misconduct and illegal activity across the nation’s largest insurance marketplace. In a newly released enforcement update, the California Department of Insurance (CDI) highlighted the scope and impact of its Investigation Division’s work as it marks its 90th year in operation. The milestone underscores how insurance fraud enforcement has evolved from basic investigations into a sophisticated system of criminal prosecution, regulatory oversight, and disaster-response protection for policyholders statewide. Why Insurance Fraud Enforcement Remains a Core Consumer Safeguard Insurance fraud affects premiums, claims processing, and consumer trust across health, auto, property, and life insurance markets. CDI investigators are tasked with identifying fraud schemes, unlicensed insurance operations, and misconduct by licensed professionals such as agents and claims adjusters. State officials emphasize that enforcement efforts are not limited to headline-making criminal cases. Everyday investigations often begin with consumer tips and lead to administrative penalties, license revocations, and industry bans that prevent future harm. How Investigators Protect Consumers During Disasters Disasters present heightened risks for fraud, particularly when displaced homeowners and small businesses urgently need insurance payments. During recent wildfire recovery operations in coastal Los Angeles County communities, investigators coordinated access for licensed adjusters into restricted areas to help accelerate claims handling. According to state data, these efforts supported billions of dollars in insurance payments and helped deter fraudulent activity targeting vulnerable disaster survivors. Investigators also took enforcement action against licensed individuals found exploiting disaster conditions, reinforcing regulatory oversight during emergency response periods. What Enforcement Results Look Like Beyond Emergencies Outside disaster response, the Investigation Division continues to pursue complex fraud cases involving premium finance abuse, life insurance misrepresentation, and unauthorized insurance activity. These cases often involve coordination with federal prosecutors and result in prison sentences, financial penalties, and long-term bans from the insurance industry. Regulators say these actions protect not only individual policyholders, but also the stability of California’s broader insurance market by removing bad actors and reinforcing compliance expectations. What the 90-Year Milestone Signals for the Future As the Investigation Division enters its tenth decade, officials stress that public participation remains essential. Many major investigations begin with consumer reports that flag suspicious activity or questionable licensing practices. State regulators continue to encourage Californians to verify licenses, report suspected fraud, and seek assistance when insurance transactions appear improper or misleading. Readers can access enforcement updates, verify licenses, or report suspected insurance fraud directly through the California Department of Insurance. FAQs: About Insurance Fraud Enforcement What does the California Department of Insurance investigate? The Department investigates insurance fraud, unlicensed insurance activity, and misconduct by licensed agents, adjusters, and other insurance professionals. How does insurance fraud impact consumers? Fraud can increase premiums, delay legitimate claims, and reduce trust in the insurance system by diverting resources away from lawful policyholders. What should consumers do if they suspect insurance fraud? Consumers should report suspected fraud to state regulators and verify whether insurance professionals are properly licensed before engaging in transactions. Why is fraud enforcement especially important after disasters? Disaster survivors are often targeted by bad actors seeking to exploit urgent insurance needs, making enforcement critical during recovery periods. Subscribe to JacobiJournal.com for trusted reporting on insurance fraud, regulatory enforcement, litigation trends, and consumer protection developments nationwide. 🔎 Read More from JacobiJournal.com:
Life Insurer Labels Kyle Busch’s $8.5M Suit ‘Inflammatory’
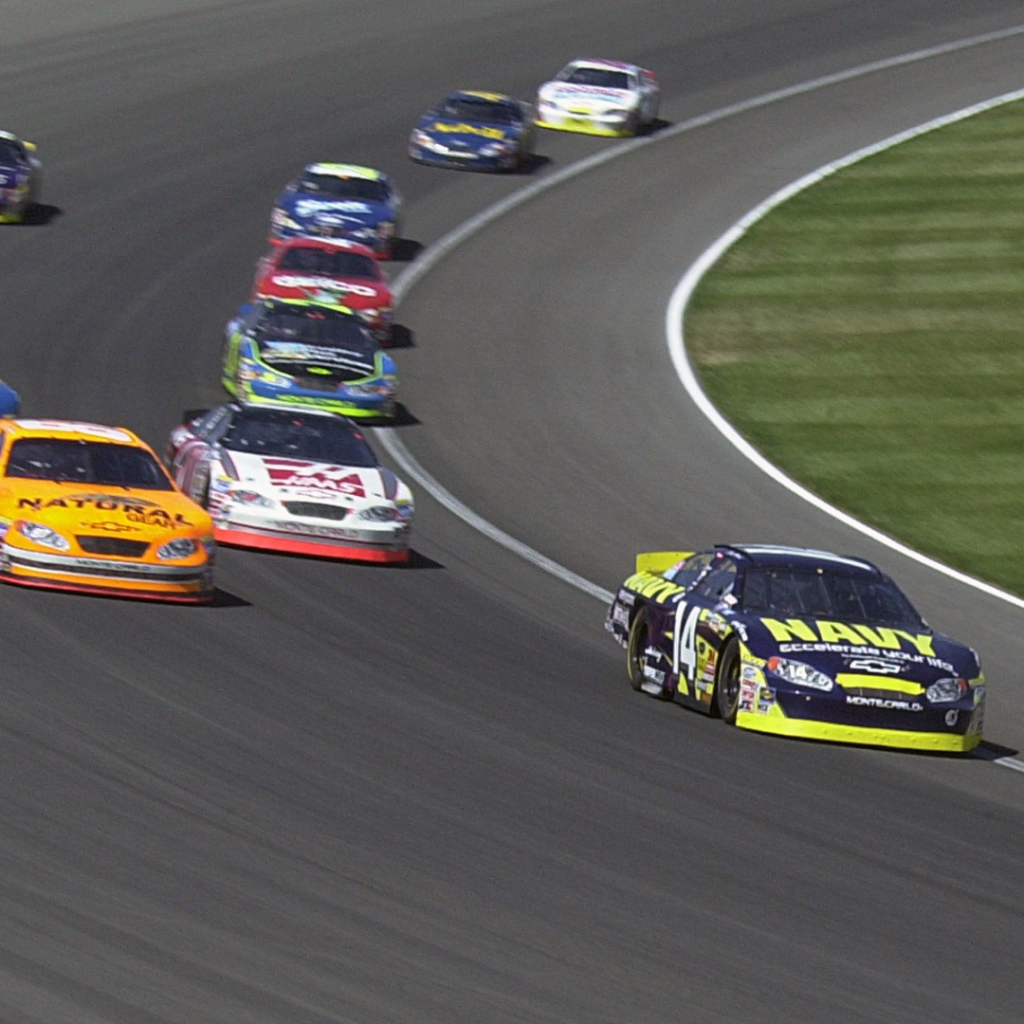
January 26, 2026 | JacobiJournal.com — A legal dispute between NASCAR driver Kyle Busch and Pacific Life Insurance Co. has taken a sharp turn, as the insurer moves to dismiss the couple’s $8.5 million lawsuit, calling the claim “inflammatory” and arguing that the policies were allowed to lapse deliberately rather than maintained for long-term growth. The lawsuit alleges the life insurance policies were “sham” agreements designed to inflate value, while Pacific Life insists the couple failed to pay premiums, leading to policy termination. The case has drawn attention for its high-profile defendant and for the broader implications it raises about insurance fraud, policy ownership, and premium responsibility. What Happened With the Policies? Pacific Life argues that Kyle Busch and his wife failed to maintain premium payments, allowing the policies to lapse. According to the insurer, this demonstrates that the policies were not treated as long-term investments, but instead were abandoned before they could grow in value. The insurer’s motion claims the couple’s lawsuit is an attempt to blame the insurance company for a self-inflicted financial decision. Why the Lawsuit Is Being Called “Inflammatory” Pacific Life’s legal filing frames the lawsuit as exaggerated and misleading. The insurer argues that the couple’s claims suggest intentional wrongdoing by Pacific Life, while the evidence shows the policies were not actively maintained. In cases like this, insurers often move to dismiss based on: The insurer’s position is that the lawsuit seeks to shift blame away from the policyholders, and that the policies were never properly sustained. How This Case Connects to Insurance Fraud Concerns This case raises questions about whether the policy was ever meant to operate as a legitimate insurance product or whether it was used for a financial strategy that failed. Insurance fraud cases often hinge on whether: If the court finds that premiums were intentionally not paid, the lawsuit could be dismissed, but if evidence suggests the insurer misled the policyholder, the case may proceed. What’s Next in the Case Pacific Life’s motion to dismiss is an early legal move designed to remove the case from court quickly. If the motion fails, the case could proceed to discovery, where both sides will produce documents, financial records, and internal communications. The outcome could influence how future insurance disputes involving high-profile individuals are handled, especially when allegations of fraud are involved. For a broader overview of how life insurance fraud claims are handled in court, readers can refer to the National Association of Insurance Commissioners (NAIC) resources on insurance fraud. FAQs: Kyle Busch Lawsuit What is Kyle Busch suing Pacific Life for? Kyle Busch and his wife claim the life insurance policies were sham agreements and are seeking $8.5 million in damages. Why is Pacific Life calling the lawsuit inflammatory? Pacific Life argues the lawsuit exaggerates the insurer’s role and claims the policies held by Kyle Busch and his wife were allowed to lapse because premiums were not paid. Can an insurance policy be considered fraud if premiums lapse? Not automatically. Courts examine intent, misrepresentation, and whether the policyholder knowingly allowed the policy to lapse. What happens if the insurer wins the dismissal motion? If the court grants Pacific Life’s motion, Kyle Busch and his wife’s lawsuit will be dismissed, and the policyholders will not receive the $8.5 million in damages they seek. Subscribe to JacobiJournal.com for timely updates on litigation, fraud cases, and major insurance disputes. 🔎 Read More from JacobiJournal.com:
INVESTIGATIVE EXCLUSIVE: RAND Study Overstates CA SIBTF Liability by $6.75 Billion

In 2022, the California DIR commissioned the RAND Corporation to review the state’s Second Injury Fund, called the Subsequent Injury Benefits Trust Fund (SIBTF), to assess its financial impact on the California Workers Compensation Industry. With it, RAND was provided unparalleled access to the state’s EMR systems. In 2024 RAND reported the results of their findings in a 180-page report. The highlight, a staggering $7.9 Billion estimated liability for the fund. This number sent shockwaves throughout the state of California and lawmakers felt the pressure to reform. A Jacobi Journal investigative report concludes that the study’s $7.9 Billion SIBTF estimate included a series of highly questionable assumptions that when put together led to a massive $6.75 billion overstatement of the fund’s future liability. RAND’s overstatement stems primarily from two critical flaws: The magnitude of the errors are so egregious that they could reasonably be considered fraudulent. It is clear to us that the specific intent of the study was to exaggerate the economic reality of California’s SIBTF liability for the purpose of bringing about a policy change at the state level. RAND’S FRAUDULENT ASSUMPTIONS 1. The study assumed 91% of all open cases would result in benefits paid to the worker when the historical average ranges from 24-44%. % of SIBTF Cases That Paid Benefits Sample Time Period Sample Size Resolved w/ Benefits All Resolved Cases 2010-2022 14,611 44.40% All Open and Closed Cases 2010-2022 27,047 24.00% RAND’s Prediction Algorithm 2019-2022 42 91.24% 2. The cost of Total Disability cases (where the applicant is found to be 100% disabled) was overstated by $453,933 per case due to several clearly false assumptions. This resulted in billions of dollars of inflated liability estimates. Assumption Error RAND’s Assumption Jacobi’s Corrected Assumption Impact on $933k Estimate Inflated COLA Rate 3.9% annual COLA 2.6% annual COLA (20-year historical average) Reduces cost to $774,017 Understated Discount Rate 3% Discount Rate 7% Discount Rate (Closer to public pension average of 6.7%) Reduces cost to $489,619 Overstated Life Expectancy General population life expectancy 17% Reduction (As admitted in RAND’s own addendum) Reduces cost to $418,345 Jacobi Corrected Estimate: Total SIBTF Future Liability = $1.25 Billion RAND study’s estimated California’s SIBTF liability to be $7.9 Billion. To arrive at that number, the study made a series of assumptions, many of which were questionable. For the purposes of simplicity we chose to focus on only two that we believed were the most impactful: the forecasted Benefit Payment Rate (91%) and the Total Cost of a Lifetime Income Award ($933,00). By simply adjusting these two factors to include assumptions that more properly reflect empirical evidence, the estimate of SIBTF liability is substantially reduced. Component RAND Study Estimate Jacobi Corrected Estimate Resolved Cases (2010-2022) $2,492,407,301 $587,450,200 Correction: Accurate Sampling Weights, COLA 2.6%, Discount Rate 7%, Corrected Life Expectancy, Reduced Life Expectancy, Sampling Adjustment Projected Unresolved Cases $5,454,644,236 $664,141,517 Corrections: Abandoned Cases Factored, Dismissal Rate of 70% used, COLA 2.6%, Discount Rate 7%, Reduced Life Expectancy Total Estimated Fund Liability $7,947,051,537 $1,251,591,717 RAND was clearly hired to produce a report to help facilitate a material alteration of the SIBTF program. To do so, they decided to manufacture a fraudulent and deceptive narrative. As a result, lawmakers in the state of California appear to be under a false assumption as it relates to the future costs related to SIBTF. We anticipate that our Investigative Report will allow lawmakers to be better informed as they evaluate the future of a benefit program that serves the severely disabled.
Funeral Director Pleads Guilty to Fraud and Mishandling Remains

November 10, 2025 | JacobiJournal.com — Funeral Director Fraud has been exposed in Hull, UK, as Robert Bush, a local funeral director, pleaded guilty on November 10, 2025, to 36 offenses including fraud and mishandling human remains. Investigations revealed that Bush accepted payments for funeral services without performing lawful burials for at least 30 deceased individuals. In multiple instances, he provided unidentified ashes to the families of stillborn babies. The case exposes serious vulnerabilities in funeral-service oversight, consumer protection, and related insurance claims. How the Fraud Occurred Authorities discovered that Bush systematically exploited grieving families by accepting payments without performing the required funeral services. His actions, which included falsifying cremation records, fabricating documentation, and providing ashes that did not belong to the deceased, are a clear example of funeral director fraud and its impact on families and the industry. What This Means for Oversight and Compliance This case underscores the importance of regulatory enforcement, audit controls, and ethical compliance in the funeral industry. Funeral homes and insurance providers should ensure: This case also highlights the need for training staff to recognize signs of misconduct and for industry leaders to establish clear reporting channels. By fostering a culture of accountability, funeral homes and insurers can reduce the risk of funeral director fraud and protect families from financial and emotional harm. Why It Matters The Bush case demonstrates the risks that arise when oversight is weak. For insurers, fraudulent funeral claims can create significant financial exposure. For regulators and consumer advocates, it underscores the importance of strict monitoring and compliance programs to prevent funeral director fraud and protect vulnerable families from both financial and emotional harm. Cases like Bush’s show that weak oversight not only harms families but also creates opportunities for funeral director fraud to go undetected. Strengthening licensing requirements, conducting regular audits, and verifying all services and payments can help prevent similar misconduct and maintain trust in the funeral industry. Learn more and read the detailed coverage here. FAQs: Funeral Director Fraud and Misconduct What crimes did the Hull funeral director commit? Robert Bush pleaded guilty to fraud and mishandling human remains, including accepting payments for services he did not perform and providing unidentified ashes to families. How did authorities uncover the fraud? Investigations were triggered by discrepancies in burial and cremation records, complaints from families, and irregularities in service documentation. Can funeral fraud affect insurance claims? Yes. Insurance providers can face financial exposure if services are misrepresented or false claims are submitted, highlighting the need for verification and auditing of claims. What steps can regulators take to prevent similar cases? Regulators can implement stricter licensing, conduct regular audits of funeral homes, enforce transparent documentation requirements, and monitor high-risk providers. Why is oversight important in the funeral industry? Weak oversight can allow unethical practices, financial exploitation of grieving families, and legal violations, making strict regulatory controls and compliance programs essential. Subscribe to JacobiJournal.com for investigative reporting on insurance fraud, compliance risks, and consumer-protection issues. 🔎 Read More from JacobiJournal.com:
Federal Judge Blocks Insurer’s Early Exit in Gas Explosion Liability Case

October 31, 2025 | JacobiJournal.com — A federal court has ruled that a major insurer must remain in a coverage dispute tied to a devastating gas explosion at an industrial site, rejecting the company’s request to withdraw before the facts of the case are fully determined. The ruling underscores how courts interpret insurance obligations when catastrophic property losses and personal injury claims arise from industrial incidents. Legal analysts note that the decision may shape how liability policies are enforced in similar high-risk situations, particularly where multiple contractors or equipment suppliers are involved. Insurer Required to Maintain Defense The case centers on a 2022 gas leak that led to a massive gas explosion, injuring several workers and destroying nearby structures. The insurer argued that the event was excluded under its policy’s hazardous-materials clause, but the court found that the underlying complaint raised potentially covered allegations — enough to require the company to stay in the case for now. “The duty to defend is triggered whenever there’s a possibility of coverage,” the judge wrote, emphasizing that insurers must remain active participants until the factual record is complete. Policy Ambiguity and Broader Industry Impact Insurance analysts say the decision could have ripple effects across the property and casualty market, especially for carriers managing industrial or construction portfolios. The ruling underscores how ambiguous exclusion language can expose insurers to extended litigation and defense costs. Legal experts also point out that courts are increasingly hesitant to grant “early exit” motions in coverage disputes involving environmental or industrial hazards, where causation often remains unclear until trial. In the aftermath of the gas explosion, both policyholder and insurer are expected to present competing interpretations of coverage terms related to negligence, equipment failure, and third-party liability. Industry observers note that these arguments often set legal precedents that shape how future catastrophic loss claims are handled under commercial general liability policies. What It Means for Policyholders For business owners, the ruling is a reminder to review policy wording carefully — particularly clauses addressing leaks, gas explosion incidents, and equipment failure. Risk managers should maintain documentation of maintenance, safety inspections, and vendor compliance to prevent coverage denials tied to alleged negligence. For more on how insurers assess catastrophic gas explosion coverage and related liability claims, see the Insurance Information Institute’s resource on liability here. FAQs: Gas Explosion Insurance Coverage Case Why did the court reject the insurer’s motion? Because the lawsuit included allegations that could fall under the policy’s general liability coverage, requiring the insurer to stay in the case. What type of policy was involved? A commercial general liability policy covering property damage and bodily injury from accidental events. How does this decision affect insurers? It limits their ability to withdraw early from complex industrial coverage disputes, forcing them to defend until facts are clarified. What should businesses learn from this? Ensure maintenance records, safety audits, and risk-management documentation are current to minimize disputes over coverage and negligence. Stay informed on coverage litigation and insurer-liability rulings — subscribe to JacobiJournal.com for weekly legal insights. 🔎 Read More from JacobiJournal.com:
NICB Reports 49% Spike in Insurance Fraud Tied to Identity Theft

October 20, 2025 | JacobiJournal.com — The National Insurance Crime Bureau (NICB) has reported a sharp 49% increase in insurance fraud cases involving identity theft and synthetic identities, marking one of the most significant fraud surges in recent years. Investigators say fraudsters are using stolen or fabricated identities to file false life insurance, healthcare reimbursement, and auto claim submissions. The trend reflects how cyber-enabled identity manipulation is fueling traditional insurance fraud schemes, often making detection harder for carriers and regulators alike. Synthetic Identities Driving Sophisticated Claim Schemes According to NICB analysts, many of the new cases involve synthetic identities—combinations of real and fake personal data used to create entirely new profiles. These synthetic claimants have been tied to false medical reimbursement requests and policies opened with fabricated beneficiaries. Experts warn that because these profiles can pass basic identity checks, insurers are increasingly vulnerable to digital-first fraud networks that exploit weak authentication processes. Life and Health Insurers See Growing Exposure Life and health insurance lines appear most affected by this year’s surge, with fraudulent actors targeting beneficiary databases and policy applications. NICB’s 2025 midyear review found that identity-based fraud has expanded from consumer policy abuse to organized criminal activity, sometimes involving multiple insurers. “These schemes often blend cybercrime with traditional claim fraud,” an NICB spokesperson said. “As digital verification expands, so does the surface area for exploitation.” Regulatory and Industry Response Emerging Regulators are responding by encouraging insurers to adopt multi-factor verification systems and cross-database fraud detection models. Insurers are also collaborating with NICB and law enforcement to share intelligence on synthetic claimants and compromised identity clusters. Industry observers predict that insurers who fail to integrate fraud analytics and biometric verification tools will face greater exposure to multi-claim identity manipulation. For the official NICB fraud trend report, visit the National Insurance Crime Bureau’s Fraud Resource Center. FAQs: Insurance Fraud Identity Theft Trends 2025 What did NICB report about identity theft and insurance fraud? NICB documented a 49% increase in insurance fraud tied to stolen or synthetic identities across multiple insurance sectors. Which types of insurance are most affected? Life and health insurance claims, along with some auto and property lines, are seeing the fastest rise in identity-linked fraud. What makes synthetic identity fraud difficult to detect? Synthetic identities blend real and fake data, often passing basic verification systems and enabling multiple false claims under different personas. How can insurers respond to this threat? Experts recommend biometric verification, AI-powered fraud analytics, and cross-industry data sharing through organizations like NICB. Stay informed on fraud enforcement and insurer liability —subscribe to JacobiJournal.com for expert weekly insights. 🔎 Read More from JacobiJournal.com:
Ameritas Urges Georgia Supreme Court To Void ‘Life Wager’ Policy

September 15, 2025 | JacobiJournal.com — Ameritas Life Insurance Corp. is pressing the Supreme Court of Georgia to rule that a controversial life insurance arrangement cannot be enforced, arguing the deal amounts to an illegal wager on human life. At the center of the dispute is an investor-backed life insurance policy that was later purchased by a trust, raising the question of whether such agreements violate Georgia’s long-standing prohibition on wagering contracts. Ameritas contends that allowing the trust to collect benefits would effectively transform life insurance into a speculative investment vehicle, undermining its intended role of providing financial security to families and policyholders. The case highlights broader concerns within the insurance industry about so-called “stranger-originated life insurance” (STOLI) policies, which regulators and courts nationwide have increasingly scrutinized for potential fraud and abuse. Insurer Challenges Investor-Backed Policy Ameritas contends that a trust holding the policy—purchased years after it was originally issued—has no legitimate right to collect death benefits. According to the insurer, such investor-driven transactions undermine the very purpose of life insurance, which is to provide financial security for families, not serve as a speculative investment vehicle. The company argues that allowing investors to profit from policies they never had an insurable interest in could open the door to widespread abuse of the insurance system. Regulators and industry groups have long warned that such practices distort the risk pool, drive up costs for legitimate policyholders, and erode public confidence in life insurance as a safety net. Ameritas maintains that if courts uphold these investor-backed arrangements, insurers may be forced to reevaluate underwriting practices and tighten compliance oversight to prevent similar disputes in the future. Stakes High for Life Settlement Industry The case is being closely watched in Georgia and beyond, as it could influence how courts treat investor-backed life settlement agreements. Industry experts warn that a ruling in favor of Ameritas could set a precedent that reshapes the market for secondary life insurance transactions. Legal observers note that these types of arrangements fall into the broader category of “stranger-originated life insurance” (STOLI), where third-party investors acquire policies with no insurable interest in the original policyholder. Courts across the country have wrestled with whether such contracts violate public policy by creating financial incentives tied to another person’s death. Ameritas argues that Georgia law, like many states, was designed to prevent such speculative practices, and the outcome of this case could set a pivotal precedent for how investor-backed life insurance is treated going forward. Broader National Trend Similar disputes have surfaced across the U.S., with insurers frequently challenging so-called “stranger-originated life insurance” (STOLI) policies. Courts have increasingly scrutinized these arrangements, questioning whether they violate long-standing public policy against wagering on human lives. In several states, high-profile rulings have either voided STOLI contracts outright or limited investors’ ability to enforce them, signaling a judicial shift toward stricter oversight. Regulators have also expressed concern that such practices could distort the life insurance market, inflating costs for policyholders who purchase coverage for legitimate family protection. Industry experts warn that unless clearer legal boundaries are established, these disputes will continue to surface, creating uncertainty for insurers, investors, and beneficiaries alike. What Comes Next in Georgia The Georgia Supreme Court’s decision will determine whether the trust may claim the policy’s benefits, or if the contract will be declared void as against public policy. A ruling is expected later this year and could have ripple effects for insurers, investors, and estate planners across the Southeast. Legal analysts note that the case could set a binding precedent in Georgia, influencing how courts in neighboring states approach similar investor-backed policies. A decision striking down the arrangement could embolden insurers to more aggressively challenge questionable policies, while a ruling in favor of the trust might encourage continued use of such structures in estate planning and investment circles. Either outcome is expected to draw close attention from financial advisors, policyholders, and lawmakers monitoring the balance between consumer protection and investment innovation in the life insurance market. For more context on life settlement regulation, visit National Association of Insurance Commissioners. FAQs: Ameritas Life Insurance Policy Georgia Ruling What is the core issue in the Ameritas case? Ameritas argues that the investor-backed life insurance policy is an illegal “wager on life” and should not be enforced. What is a STOLI policy? A STOLI, or stranger-originated life insurance policy, involves investors purchasing life insurance on strangers, often raising public policy concerns. Why does this case matter beyond Georgia? The ruling could influence national treatment of investor-backed life settlements, shaping future litigation and regulatory approaches. When is a decision expected? The Georgia Supreme Court is reviewing arguments now, with a ruling anticipated before the end of 2025. Subscribe to JacobiJournal.com for timely updates on insurance litigation and financial fraud cases. 🔎 Read More from JacobiJournal.com:
Second Circuit Orders Resentencing in $600M Medical Billing Fraud Case

September 12, 2025 | JacobiJournal.com — A federal appeals court has affirmed the conviction of a Long Island medical biller who orchestrated a $600 million medical billing fraud scheme but sent the case back to the trial court for resentencing. The ruling underscores the judiciary’s continued focus on accountability in one of the largest medical billing fraud cases ever prosecuted. Conviction Upheld, But Sentencing Reconsidered The Second Circuit panel ruled that the evidence of fraud was overwhelming, leaving no question about the defendant’s guilt. However, the court determined that errors in the original sentencing required the case to be remanded for further review. The decision leaves the conviction intact while opening the door for a new assessment of the punishment. $600 Million Fraud Scheme Detailed According to federal prosecutors, the biller submitted fraudulent insurance claims totaling hundreds of millions of dollars and went so far as to impersonate professional athletes, including an NBA player and NFL figures, to further the scheme. The elaborate fraud exploited weaknesses in the medical billing system, resulting in one of the largest recoveries ever pursued in a single case. Broader Implications for Health Care Fraud Enforcement Legal analysts say the ruling highlights the importance of strong sentencing procedures in health care fraud cases. It also reinforces the government’s aggressive stance against schemes that threaten the stability of insurance systems and increase costs for policyholders nationwide. With medical billing fraud continuing to rise, this case may set a standard for future prosecutions. For official documentation and case details, readers can review filings at the U.S. Court of Appeals for the Second Circuit. FAQs: $600M Medical Billing Fraud Case What was the fraud about? The defendant submitted fraudulent insurance claims worth approximately $600 million, using false identities and impersonations to support the scheme. What did the Second Circuit decide? The appeals court affirmed the conviction but remanded the case for resentencing due to procedural errors in the original judgment. Why is resentencing significant? It ensures sentencing procedures meet federal standards, giving the defendant a fair hearing while maintaining accountability for large-scale fraud. How does this affect future health care fraud cases? The ruling reinforces both the seriousness of medical billing fraud and the need for careful sentencing, likely influencing how future fraud prosecutions are handled. Stay informed on major insurance fraud and health care litigation by subscribing to JacobiJournal.com. 🔎 Read More from JacobiJournal.com: